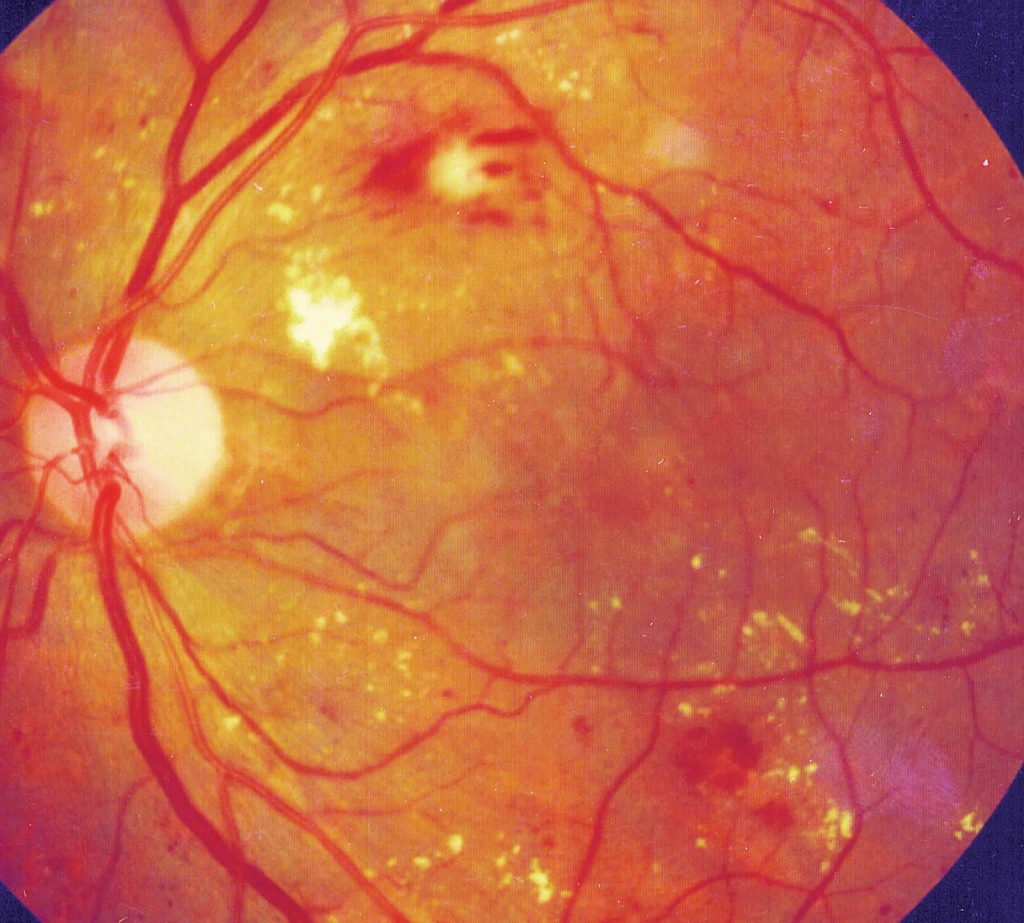
(Diabetic macular oedema and Diabetic Retinopathy)
In principle, the eye is very similar in design to a camera. When you look at an object, the light from the object passes through your pupil and is focused by the natural lens in your eye onto the retina, in exactly the same way as a camera lens focuses light onto a film in the camera.
The retina has two essential parts, the peripheral retina responsible for night vision and side vision, and the macula, responsible for fine vision i.e. looking at a car number plate in the distance and reading close-up. The macula is very small, only the size of a pinhead but is critical for your fine vision.
For the retina to function normally it requires a blood supply, one artery enters the eye, divides into four smaller arteries and subsequently into many small capillaries that supply blood and oxygen to the retina.
Over many years diabetes damages the tiny capillary blood vessels in the retina to make them leaky or to block them altogether. If blood vessels in the macula block completely, called macular ischaemia, this will have an effect on vision and is untreatable. However, it is much more common that people develop leaky blood vessels affecting the centre of the macula, as a result of diabetes for many years.
When fluid leaks out of capillary vessels into the macula itself, the macula swells and the vision becomes blurred and often distorted. If left untreated, the situation gradually gets worse, eventually leading to irreversible poor vision.
It’s rare that patients sense any change in vision unless the disease is moderately advanced, and that is why patients with diabetes need to have regular eye examinations and retinal imaging.
Symptoms may include:
Talk with Prof. Michel if you have any of these symptoms right away.
With a comprehensive eye examination, including a retinal examination and detailed retinal imaging after dilating eye drops have been instilled. It is the best way to check for eye problems from diabetes.
Prof. Michel will also:
In short, yes. But in certain situations! Before ten years ago, the only treatment available for this was macular laser therapy. This treatment was effective at reducing the risk of visual deterioration by 50-60%, but essentially did not improve vision. In certain situations, where leakage of fluid occurs off-centre, i.e. eccentrically, so that the very centre of the macula is not involved, it is appropriate to treat this with laser therapy.
However, if macular oedema involves the centre of the macula, then treatment with anti-VEGF therapy injections into the eye is required. Macular oedema and macular ischaemia are often together termed diabetic maculopathy.
It is essential to maintain a good control of your underlying diabetes hypertension and any abnormal lipid levels, as the first step in managing your diabetic maculopathy. Studies showed that patients in which these factors are well-controlled have a very significantly reduced risk of developing macular oedema or any form of diabetic eye disease in the first place and of it progressing if they do develop it.
Once macular oedema does occur and involves the central vision, anti-VEGF therapy with one of three agents, Eylea (Aflibercept), Lucentis (Ranibizumab) or Avastin (bevacizumab) is required.
Extensive clinical trials have been performed using these drugs and essentially show that they will stabilise visual acuity, i.e. prevent deterioration of vision in 95% of patients who take them on a regular basis. In addition, patients will achieve a three-line improvement in visual acuity in approximately a third of cases, and a two-line gain in vision in about 50% of cases.
The treatment is not a single injection, it involves a regular course of injections that can last for a number of years. On average, patients in clinical studies were taking 7 to 8 injections in year one, 4 to 6 in year two, 2 to 3 in year three, 1 to 2 in year four and 1 in year five. However, these figures represent a guideline only and some patients, particularly if their diabetes and blood pressure is under excellent control, will require less, and others in whom the control could be improved, will require more.
In terms of the three drugs, a clinical trial performed in the United States, called Protocol T, showed that there were small differences between the drugs. At two years there was no significant difference between Lucentis and Eylea in the amount in which they improved vision; but these two drugs were slightly better than Avastin, particularly in patients with less good baseline visual acuity. The study showed that patients gained approximately 2 letters more i.e. less than half a line of vision (each line on a visual acuity chart contains five letters) with Eylea and Lucentis, compared to Avastin. They were also slightly more effective in drying out or reducing the fluid in the centre of the macula than Avastin.
However, two letters of visual acuity difference is very small and would not be noticed by the majority of patients, and some have questioned; therefore, whether this represents a meaningful clinical difference. In essence, Eylea and Lucentis are approved treatments for the condition, and Avastin is used as an off-label i.e. officially unapproved but significantly cheaper alternative option. The side-effect profiles of the drugs used in Protocol T were essentially the same.
Prof. Michel is currently performing the injections at The London Medical in a dedicated intraocular injection room on Mondays all day and Thursdays from 2pm onwards. Please arrive 30 minutes before your injection time. A nurse will measure your visual acuity, intraocular pressure and insert pupil dilating drops and likely perform an OCT scan, i.e. high-resolution 3D image of the centre of the retina, the macula. Prof. Michel will see you immediately before the injection, administer anaesthetic drops, check clinical findings and answer questions etc.
The injection itself involves you lying down on a couch in the dedicated injection room for ten minutes. During this time, Prof. Michel will scrub up, put on sterile gloves and gown, sterilise around the eye with a solution of iodine, and perform the injection – which takes less than 5 seconds and which you will hardly notice. You may be aware of a light being shone into the eye at the end of the procedure which is done to check inside the eye.
After each injection, the eye will be a little tender for a few hours, and you may experience a few floaters, and occasionally a small bubble at the bottom of your visual field in the injected eye.
These are expected and typically settle over 24 hours. Antibiotic drops are not routinely given after injection as evidence suggests they may slightly increase the risk of infection in the eye. You will, however, be given lubricant drops in case the eye feels dry or irritable post-injection.
Prof. Michel or his secretary will contact you approximately three days after the procedure to check that everything has settled well and that you have no untoward symptoms.
If you note the onset, often quite rapidly, of blurred vision, increasing redness, pain or light sensitivity in the injected eye, at any time after the injection, but particularly in the first 72 hours, please make contact immediately.
The main risk of the treatment is approximately 1 in 1000 risk of infection in the eye with each injection which could significantly affect vision or even lead to complete loss of vision if it did occur. Whilst this is, therefore, a very unlikely event, please follow carefully the instructions given to you when beginning treatment and please see the advice sheet ‘Intravitreal injection’[M1] . This gives specific instructions on looking out for any signs of infection in the eye and what to do if you think this may have occurred.
Whilst having injections for diabetic macular oedema, it is still important that the severity of retinopathy that you have affecting the peripheral retina is monitored.
This retinopathy can also be helped or stabilized as a beneficial side-effect of the anti-VEGF therapy injections, but it is possible that during your injection treatment for diabetic macular oedema, pan-retinal photocoagulation (peripheral laser therapy) will be necessary for proliferative diabetic retinopathy.
In addition, patients may develop cataract during treatment of diabetic maculopathy as this is more likely in diabetic patients anyway and it may be that cataract surgery will need to be performed at some stage, but Prof. Michel will advise you if this is the case.
Your message has been sent. We will get back to you.